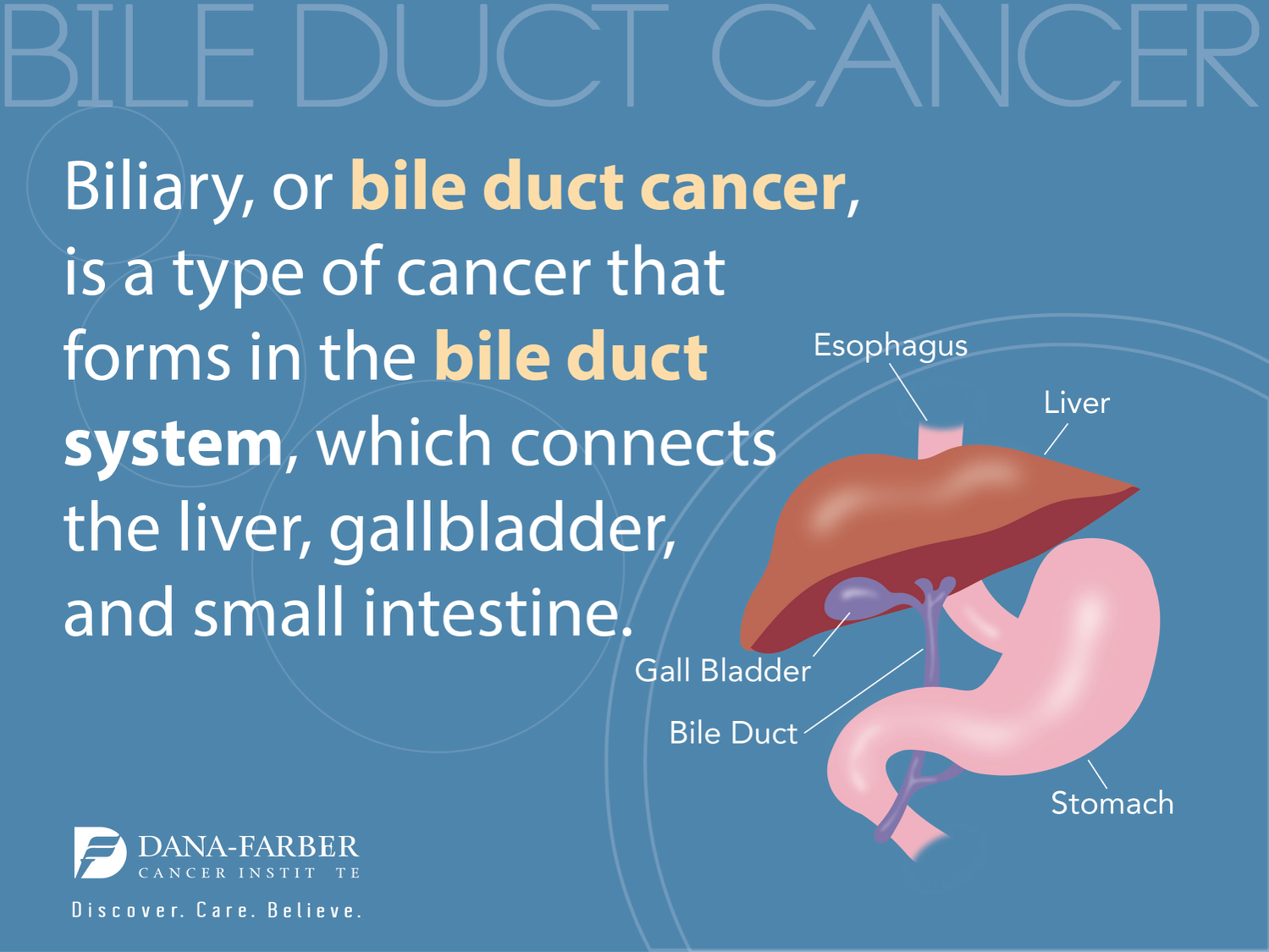
Pediatric cancer relapse prediction has taken a significant leap forward with the advent of artificial intelligence in cancer care. A groundbreaking study from Mass General Brigham revealed that an AI tool outperforms traditional methods in forecasting the recurrence risk for children diagnosed with brain tumors, particularly pediatric gliomas. By analyzing longitudinal brain scans, the AI employed innovative techniques like temporal learning to provide earlier warnings about potential relapses, thereby enhancing treatment decisions and patient care. Predicting recurrence risk with such high accuracy—between 75-89%—transforms how clinicians approach brain tumor treatment, promising less stress for young patients and their families. This advancement not only highlights the role of AI in reshaping pediatric oncology but also paves the way for a future where personalized medicine can directly impact survival outcomes.
In the realm of childhood cancers, predicting the likelihood of tumor recurrence is crucial for ensuring effective treatment strategies. Various technological advancements, particularly in the field of artificial intelligence, are revolutionizing the understanding of pediatric oncological conditions, including brain tumors like pediatric glioma. Leveraging AI’s capabilities allows healthcare professionals to assess recurrence risk through comprehensive analyses of multiple imaging scans over time. Such predictive models can greatly influence management decisions, optimizing care for survivors by reducing unnecessary interventions while addressing high-risk patients more proactively. The ongoing integration of sophisticated machine learning techniques and temporal learning methodologies into cancer care signifies an exciting shift towards enhanced therapeutic precision and patient outcomes.
The Role of AI in Pediatric Cancer Care
Artificial Intelligence (AI) is revolutionizing pediatric cancer care by enhancing predictive accuracy and treatment plans. One remarkable application is the advanced AI tools used to predict the likelihood of cancer relapse in young patients. These innovations leverage vast datasets, facilitating a deeper understanding of factors influencing pediatric glioma outcomes. Traditional methods often rely on limited imaging results, while AI, particularly through temporal learning techniques, utilizes a series of scans to provide a comprehensive analysis of a child’s health over time.
The integration of AI in medical practice not only promises improved accuracy but also alleviates some burdens from families dealing with pediatric cancer. By offering more precise predictions regarding the recurrence risk of brain tumors, medical teams can tailor follow-up care and necessary interventions more effectively. This proactive approach helps minimize unnecessary anxiety and medical procedures for patients, ensuring they receive only the most relevant and beneficial care.
Pediatric Cancer Relapse Prediction: A Game Changer
The innovation in pediatric cancer relapse prediction derived from AI technology marks a significant leap forward in pediatric oncology. By analyzing longitudinal MRI scans, researchers have improved the accuracy of predicting recurrence in pediatric glioma cases, achieving results that far surpass those obtained through traditional single-scan evaluations. This demonstrates a shifting paradigm where patients can be categorized by their risk levels much more efficiently, allowing for timely interventions when necessary.
The implications of these predictive capabilities are profound. For families, having a clearer picture of the risk profile can guide them through complex decisions regarding treatment options and follow-ups. Furthermore, reducing the frequency of scans for low-risk patients has the potential to enhance quality of life, both psychologically and physically. Equally, high-risk patients can receive immediate, targeted treatments that address their specific needs, fostering a more personalized approach to pediatric brain tumor treatment.
Temporal Learning AI in Pediatric Oncology
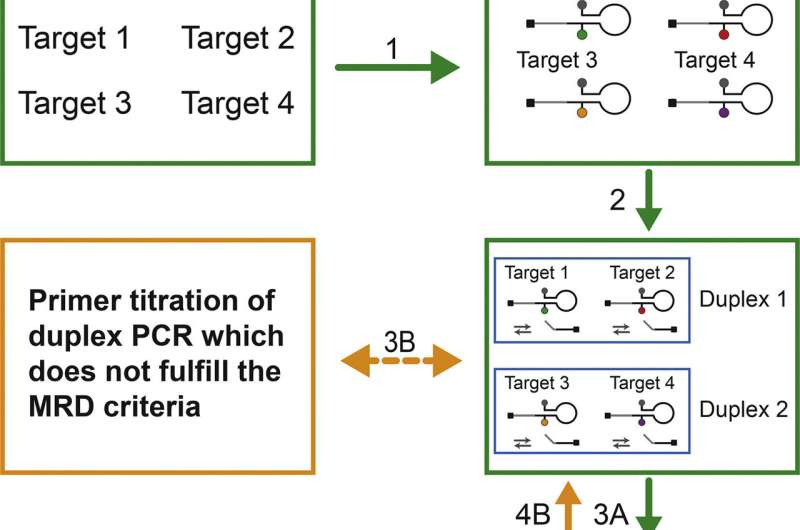
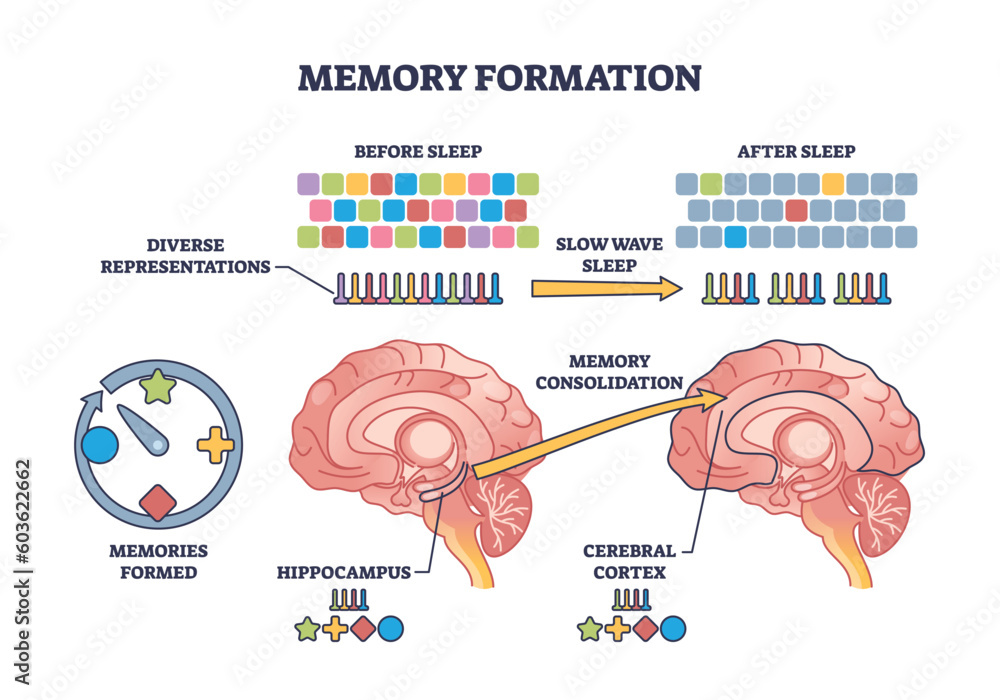
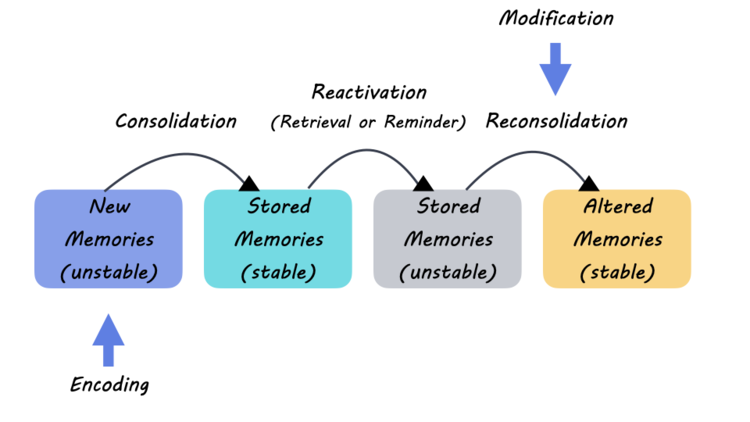
Temporal learning, an advanced AI technique utilized in recent studies, highlights how data can be interpreted over time for better predictive outcomes. Instead of relying solely on static images from a single moment, this innovative method enables the AI to process sequences of MRIs, thereby detecting subtle changes in the brain that could indicate potential relapse. The ability to recognize trends across multiple timepoints represents a crucial advancement in the fight against pediatric gliomas.
This approach not only enhances the predictive capabilities of AI but also underscores the importance of comprehensive monitoring throughout a patient’s recovery journey. By offering a richer dataset, temporal learning helps healthcare providers make more informed decisions, improving the overall efficacy of brain tumor treatment. It exemplifies how AI can transform the landscape of cancer diagnostics, pushing boundaries to ensure that children receive the most effective care possible.
Improving Care with AI in Brain Tumor Treatment
Incorporating AI tools into pediatric oncology has the potential to redefine patient care standards. Specifically, when dealing with diseases like pediatric gliomas, where treatment must be both aggressive and careful, AI-driven insights ensure that children receive personalized attention. Such innovations lead to earlier interventions based on accurate assessments of recurrence risk, fostering a treatment environment that prioritizes patient well-being.
The shift towards AI-guided treatment plans signifies a broader evolution in how we approach childhood cancers. By prioritizing predictive analytics, healthcare providers can create streamlined protocols that not only target the disease more effectively but also lessen the psychological and physical toll on pediatric patients. These advancements represent a significant step towards a future where treatment is not only reactive but proactive, ultimately enhancing survival rates and life quality for children battling brain tumors.
Future Directions in Pediatric Cancer Research
As research continues to evolve, the integration of AI in predicting pediatric cancer outcomes is still in its early stages, yet the potential is enormous. Future studies are anticipated to focus on further validating AI models across diverse populations and settings, ensuring that these tools are robust and applicable to various clinical scenarios. This validation process will be crucial in establishing trust and reliability in AI applications for pediatric gliomas.
Additionally, the exploration of AI’s capabilities will likely extend beyond just prediction models into treatment recommendations and risk assessment frameworks. The intersection of AI and pediatric oncology holds the promise of a future where every child battling cancer can receive customized treatment pathways backed by statistical insights, ultimately moving us closer to personalized medicine. Collaborative efforts across institutions will play a pivotal role in this endeavor, fostering innovation and transformation in pediatric cancer care.
Challenges in Implementing AI for Cancer Predictions
Despite the promising advancements in AI technology for predicting pediatric cancer relapse, several challenges remain. The healthcare industry must address issues related to data privacy, regulatory compliance, and ethical considerations around AI deployment in clinical settings. It is imperative to ensure that AI algorithms are not only effective but also transparent and explainable to healthcare providers and patients alike.
Moreover, integrating AI tools into existing healthcare infrastructure can be met with resistance due to differing levels of technology adoption across facilities. Training healthcare staff to utilize these tools effectively will be critical for maximizing the benefits of AI in pediatric oncology. Continuous education and resource allocation will enable a smoother integration of these technologies, ensuring that the fight against pediatric brain tumors can fully harness the potential of AI.
Longitudinal Imaging and Its Impact on Recurrence Rates
Longitudinal imaging plays a pivotal role in monitoring pediatric gliomas and understanding recurrence patterns. By frequently analyzing multiple MRIs over extended periods, clinicians can observe changes that might indicate a potential relapse before it manifests clearly. This proactive monitoring can significantly alter the course of treatment, leading to timely interventions that could enhance patient outcomes.
Moreover, longitudinal studies contribute to building a larger data set that can be used for refining AI models. As researchers gather more imaging data throughout the treatment journey, they can improve the algorithms’ predictive accuracy, contributing to a deeper understanding of how pediatric cancers behave over time. This continuous cycle of observation and adaptation ultimately leads to advancements in treatment strategies and better survival rates for young patients.
The Importance of Family Involvement in Pediatric Cancer Treatment
Family involvement is crucial in pediatric cancer treatment, influencing both the emotional and psychological well-being of children battling gliomas. Educating families about the potential risks of recurrence and the role of AI in monitoring their child’s health can empower them to engage more actively in the treatment process. By understanding the intricacies of their child’s condition, families can provide essential support and advocacy.
Moreover, the integration of AI predictions concerning recurrence risk into discussions with families can help set realistic expectations regarding follow-up care. This collaborative approach not only alleviates anxiety but also allows for better planning and prioritization of resources, ensuring that families remain informed and invested in their child’s treatment plan. The emotional resilience fostered through family involvement is an invaluable component of successful pediatric oncology.
AI Innovations in Imaging Technology
The evolution of imaging technology, coupled with AI advancements, represents a transformative trend in pediatric cancer diagnostics. Enhanced imaging techniques such as MRI offer clearer pictures of brain tumors, while AI algorithms analyze these images with unprecedented precision. This combination contributes greatly to the accuracy of tumor assessments and the prediction of recurrence risk, allowing for proactive management of pediatric gliomas.
As imaging technology continues to advance, the partnership with AI will likely yield novel insights into tumor behavior, recurrence patterns, and treatment responses. The focus on developing cutting-edge imaging solutions ensures that clinicians have the best tools at their disposal for monitoring changes and making informed treatment decisions. This partnership heralds an exciting future where technology serves as a cornerstone in the fight against pediatric cancer.
Frequently Asked Questions
How does AI improve pediatric cancer relapse prediction for brain tumors?
AI enhances pediatric cancer relapse prediction, particularly for brain tumors like gliomas, by utilizing advanced techniques such as temporal learning. This approach analyzes multiple brain scans over time, allowing for more accurate evaluations of recurrence risk compared to traditional methods. By recognizing subtle changes across scans instead of relying on a single image, AI can predict relapse with an accuracy of 75-89 percent.
What role does temporal learning play in predicting pediatric glioma relapse?
Temporal learning plays a crucial role in predicting pediatric glioma relapse by training AI models to analyze a sequence of post-surgery MRI scans. This method helps the AI recognize patterns and changes over time, significantly improving the prediction of recurrence risk. Unlike conventional models that focus on individual scans, temporal learning allows for a comprehensive assessment, leading to better-informed treatment strategies.
Why is it important to predict recurrence risk in pediatric cancer patients?
Predicting recurrence risk in pediatric cancer patients, such as those with gliomas, is essential for optimizing treatment and improving quality of life. Accurate predictions enable healthcare providers to tailor follow-up care, potentially reducing the frequency of stress-inducing imaging sessions while ensuring high-risk patients receive timely interventions. This personalized approach can enhance overall patient outcomes.
What is the significance of the accuracy achieved by AI in pediatric cancer relapse prediction?
The AI’s accuracy in pediatric cancer relapse prediction, ranging from 75-89 percent, represents a significant advancement over traditional approaches, which often show around 50 percent accuracy based on single images. This improvement means better risk assessment for children with brain tumors, allowing for more proactive and targeted treatment plans. Enhanced predictive capabilities can lead to more effective care and improved long-term outcomes.
What potential future applications does this AI technology have in pediatric cancer care?
This AI technology, particularly through its temporal learning approach, has the potential to revolutionize pediatric cancer care by enabling precise predictions of relapse for various conditions beyond gliomas. Future applications may include reducing unnecessary imaging for low-risk patients and guiding adjuvant therapy decisions for high-risk cases. Continued development and validation in clinical settings could pave the way for broader implementation in pediatric oncology.
How can families benefit from advancements in pediatric cancer relapse prediction using AI?
Families can benefit significantly from advancements in pediatric cancer relapse prediction using AI by experiencing reduced anxiety and burden associated with frequent imaging. With improved predictive tools, care options become more tailored, allowing families to focus on supporting their child’s recovery rather than worrying about potential relapses. Ultimately, this leads to a more positive healthcare experience for both patients and their families.
| Key Points |
|---|
| An AI tool significantly improves prediction of pediatric cancer relapse compared to traditional methods. |
| Utilizes temporal learning by analyzing multiple brain scans taken over time post-surgery. |
| Achieved 75-89% accuracy in predicting recurrence of gliomas within one year after treatment. |
| Highlight the difficulty in predicting recurrence, necessitating more advanced tools for patient care. |
| The approach may lead to tailored treatments based on patient risk levels. |
Summary
Pediatric cancer relapse prediction is crucial for improving outcomes in young patients. Recent advances show that AI tools, particularly those employing temporal learning techniques, can accurately forecast the risk of cancer recurrence in pediatric patients with gliomas far better than traditional methods. This revolutionary approach not only enhances prediction accuracy but also aims to relieve the stress of frequent imaging follow-ups for families. With the potential for tailored treatment plans based on individual risk, this study underscores an exciting advancement in pediatric oncology that could reshape care for children battling cancer.