Pediatric brain cancer AI is transforming the landscape of oncology for young patients, particularly those diagnosed with gliomas. In a groundbreaking study, researchers harnessed the power of artificial intelligence to analyze brain scans over time, predicting the risk of cancer relapse with impressive accuracy compared to traditional methods. This innovative AI tool could significantly change the management of pediatric brain cancer by facilitating earlier detection of patients at high risk for relapse, thus ensuring timely interventions. The integration of temporal learning techniques allows the model to consider historical imaging data, enhancing its predictive capabilities. By doing so, pediatric brain cancer AI promises to not only improve survival rates but also alleviate the burdensome follow-up protocols that currently stress children and their families.
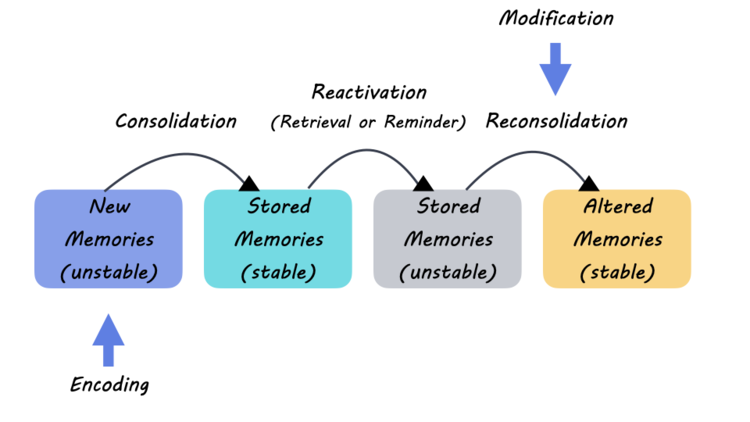
AI applications in pediatric oncology represent a crucial advancement in treating childhood tumors, specifically focusing on brain malignancies. Leveraging cutting-edge technology, these tools can effectively monitor ongoing patient health and assess the likelihood of brain cancer relapse, which is vital for timely treatment adjustments. The study highlights the significance of utilizing temporal learning in machine learning, allowing the AI to comprehensively analyze changes across a series of MR scans, ultimately enhancing glioma treatment strategies. By exploring the potential of radiation oncology AI, medical professionals hope to streamline patient care and focus on high-risk cases, thus optimizing both outcomes and overall resource allocation.
The Role of AI in Predicting Pediatric Brain Cancer Relapse
Recent advancements in artificial intelligence (AI) have significantly transformed the landscape of pediatric oncology, particularly in the management of brain cancers like gliomas that are prevalent among children. The study conducted by researchers at Mass General Brigham demonstrated that an AI tool trained on numerous MRI scans is capable of predicting the risk of cancer relapse much more reliably than traditional methods. This innovation marks a milestone in pediatric brain cancer AI, as it not only enhances diagnostic accuracy but also alleviates the emotional and physical burden on young patients and their families during the follow-up period.
By utilizing AI to analyze multiple timelined brain images, the researchers can detect subtle changes in tumor characteristics that may indicate an impending relapse, a feat that traditional single-scan assessments often fail to accomplish. This advancement not only provides a more accurate prediction of recurrence but potentially reduces the frequency of invasive imaging procedures that many patients undergo, thus paving the way for a tailored treatment plan that focuses on individual patient risks.
Frequently Asked Questions
What is the role of AI in pediatric brain cancer diagnosis and treatment?
AI in pediatric oncology enhances the accuracy of brain cancer diagnosis and treatment by analyzing vast amounts of data, including brain scans. Utilizing advanced techniques like temporal learning, AI can predict the risk of brain cancer relapse more reliably than traditional methods, aiding in personalized treatment plans for young patients.
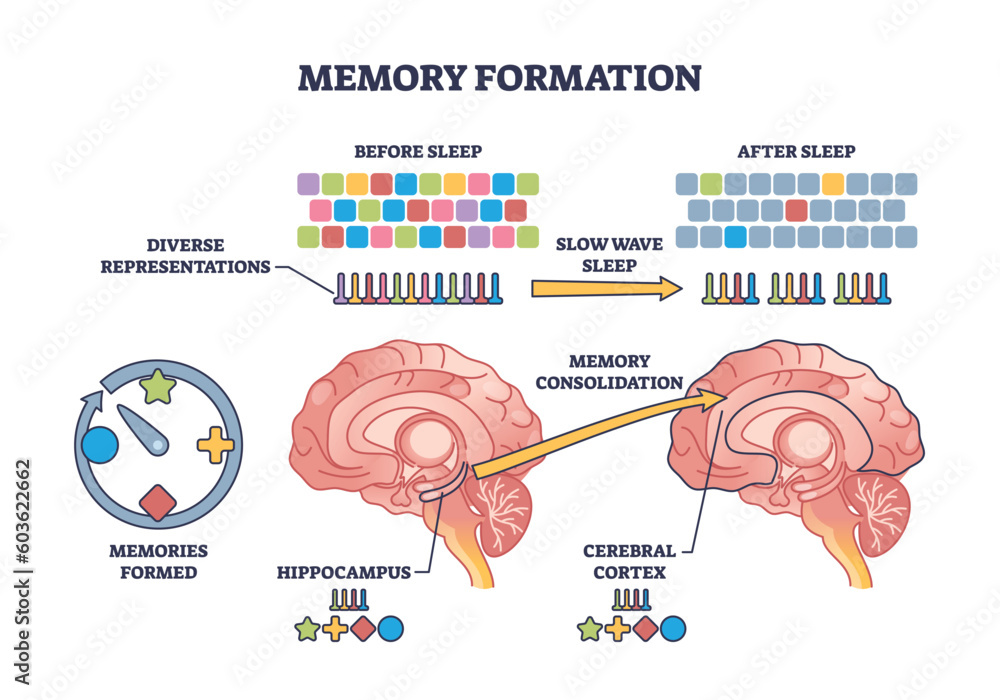
How does temporal learning improve predictions of glioma treatment outcomes?
Temporal learning, a pivotal technique in pediatric brain cancer AI, improves glioma treatment outcome predictions by analyzing multiple brain scans over time. This approach allows the AI model to recognize subtle changes that may indicate a risk of relapse, leading to earlier interventions and better patient management.
What are the benefits of using AI for predicting brain cancer relapse in children?
The benefits of using AI for predicting brain cancer relapse in children include increased accuracy in risk assessment, reduced need for frequent imaging, and personalized treatment strategies. By predicting relapse more effectively, AI can help clinicians determine which patients require closer monitoring or proactive treatments.
Can AI tools effectively identify high-risk pediatric patients for brain cancer?
Yes, AI tools are proven to effectively identify high-risk pediatric patients for brain cancer. Through the application of temporal learning in analyzing post-surgery MR scans, AI can detect early signs of tumor recurrence, hence enabling timely decisions regarding patient care and treatment adjustments.
What advancements have been made in radiation oncology AI for treating pediatric brain cancer?
Advancements in radiation oncology AI for treating pediatric brain cancer include the development of models that integrate historical imaging data and predict patient outcomes with greater accuracy. These innovations assist clinicians in tailoring radiation treatments to improve the efficacy and safety for young patients.
How does AI in pediatric oncology enhance the understanding of glioma progression?
AI in pediatric oncology enhances the understanding of glioma progression by utilizing machine learning techniques to analyze patterns from sequential brain scans. This comprehensive analysis helps to reveal the dynamic nature of tumor growth and potential recurrence, offering insights that guide treatment decisions.
Are there any clinical trials involving pediatric brain cancer AI on the horizon?
Yes, there are plans to initiate clinical trials investigating the application of pediatric brain cancer AI in predicting relapse and informing treatment pathways. These trials aim to validate the effectiveness of AI-informed risk assessments in improving clinical outcomes for children with brain tumors.
What challenges are faced in implementing AI for pediatric brain cancer risk prediction?
Challenges in implementing AI for pediatric brain cancer risk prediction include the need for further validation in diverse clinical settings, ensuring data privacy, and integrating AI insights into existing healthcare workflows. Addressing these challenges is crucial for realizing the full potential of AI in pediatric oncology.
| Key Point | Details |
|---|---|
| AI Tool Predicts Relapse | A new AI tool analyzes brain scans over time to predict relapse in pediatric glioma patients more accurately than traditional methods. |
| Importance of Early Detection | Early relapse detection can improve treatment outcomes and reduce distress for children and families. |
| Temporal Learning Technique | Uses multiple brain scans over time to recognize subtle changes, enhancing predictive accuracy. |
| Study Collaboration | Conducted by Mass General Brigham, Boston Children’s Hospital, and Dana-Farber, it analyzed nearly 4,000 MR scans from 715 patients. |
| Prediction Accuracy | The AI model achieved a 75-89% accuracy in predicting glioma recurrence, significantly better than the 50% accuracy from single images. |
| Next Steps | Further validation is needed, and clinical trials may explore AI-informed predictions for patient care adjustments. |
Summary
Pediatric brain cancer AI offers transformative potential by predicting relapse risks more accurately than traditional methods. This new study showcases how AI tools trained on multiple brain scans can lead to timely interventions for pediatric glioma patients, ultimately improving treatment strategies and reducing anxiety for affected families. By harnessing the power of temporal learning, researchers highlight a promising path forward in pediatric oncology.