Pediatric cancer recurrence is a critical area of concern, especially for children diagnosed with brain tumors such as gliomas. Recent advancements in AI in pediatric oncology have opened new pathways to better predict relapse risks, significantly enhancing patient care. A study from Mass General Brigham has shown that an AI tool analyzing multiple MRI scans can forecast recurrence more accurately than traditional methods, thereby alleviating some of the stresses associated with frequent follow-ups. The innovative approach utilizes machine learning cancer diagnosis techniques to identify subtle changes in tumor behavior over time. By leveraging temporal learning in medicine, researchers aim to revolutionize how pediatric cancer recurrence is monitored, offering hope for improved outcomes for young patients.
The recurrence of cancer in children, particularly after initial treatment, remains a daunting challenge for families and healthcare professionals alike. This condition, often linked to specific tumor types like gliomas, warrants early detection and intervention strategies. Researchers are now turning to cutting-edge technologies such as artificial intelligence and machine learning, which have the potential to transform cancer management. For instance, enhanced MRI scans in pediatric patients allow for a more dynamic assessment of tumor progression, leading to timely therapeutic decisions. By adopting innovative approaches like temporal learning, the medical community aims to refine our understanding of relapse risks in pediatric oncology.
Advancements in AI for Pediatric Cancer Diagnosis
The integration of artificial intelligence (AI) into pediatric oncology marks a significant stride in the early detection and management of childhood cancers. Recent studies have demonstrated how AI tools enhance the diagnostic process, yielding insights that surpass traditional methodologies. Such advancements are particularly crucial in analyzing complex data, such as MRI scans for pediatric cancer patients, providing oncologists with deeper understanding and improved decision-making capabilities.
Moreover, machine learning algorithms are being increasingly utilized to scrutinize various parameters in cancer diagnosis, allowing medical professionals to identify patterns that are often overlooked in standard evaluations. The incorporation of AI in pediatric oncology is not just about making accurate diagnoses; it is also about optimizing treatment plans based on data-driven predictions and assessments that can ultimately improve patient outcomes.
The Role of Temporal Learning in Predicting Cancer Recurrence
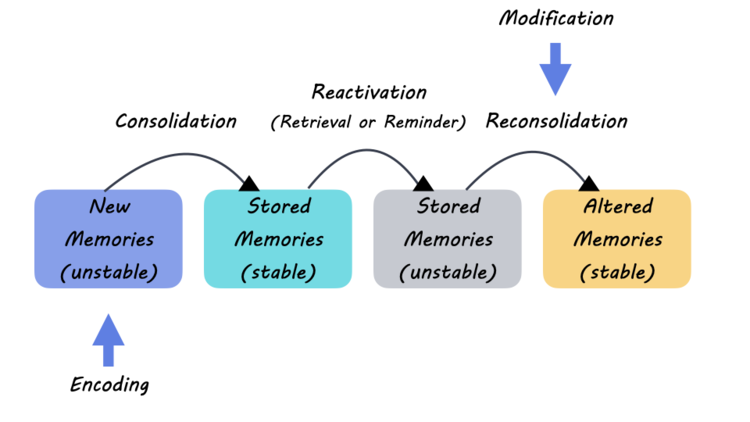
Temporal learning has emerged as a groundbreaking approach in predicting cancer recurrence, particularly in pediatric patients with gliomas. Instead of relying on individual scans taken at isolated points in time, this innovative technique analyzes a series of MRI scans over an extended period. By doing so, it captures the nuanced changes in tumor dynamics that may indicate potential recurrence, leading to more precise evaluations regarding a patient’s prognosis.
This temporal learning method facilitates the synthesis of information from multiple imaging sessions, effectively training AI models to recognize subtle shifts that traditional analysis might miss. The findings from recent research show that employing this method can significantly enhance the accuracy of glioma recurrence predictions, affording both physicians and families improved foresight regarding treatment and follow-up plans.
Understanding Glioma Recurrence through AI Tools
Gliomas, which represent a significant portion of pediatric brain tumors, often pose challenges in terms of their unpredictable nature and propensity for recurrence. The latest advancements in AI technology have provided researchers with tools that enhance the understanding of glioma behavior over time. By analyzing patterns in MRI scans, AI models can identify factors that correlate with recurrence, thus providing critical insights into patient management.
These AI-driven approaches not only aim to improve the accuracy of recurrence predictions but also have the potential to influence treatment protocols. For instance, identifying high-risk patients earlier can lead to tailored adjuvant therapies that may mitigate the chances of relapse and optimize long-term outcomes for pediatric cancer patients.
The Impact of Machine Learning on Pediatric Oncological Care
Machine learning is transforming pediatric oncological care by fostering an environment where data-driven decisions can be made swiftly and accurately. For pediatric patients diagnosed with cancers such as gliomas, machine learning algorithms can process extensive medical records and imaging data to discern patterns that inform clinical strategies. This shift towards evidence-based care models not only enhances diagnostic precision but also empowers clinicians to personalize treatment plans that cater to individual patient needs.
As researchers continue to refine machine learning techniques within pediatric oncology, the implications for patient outcomes are profound. With an increasing amount of healthcare data at their disposal, healthcare providers can rely on automated systems to forecast disease trajectories, thereby improving surveillance protocols and tailoring interventions that preemptively address the risk of recurrence.
MRI Scans: A Vital Tool in Pediatric Cancer Monitoring
Magnetic resonance imaging (MRI) scans are indispensable assets in the monitoring of pediatric cancer patients. These non-invasive imaging tools enable oncologists to visualize tumor growth and determine the effectiveness of ongoing treatments. For pediatric patients, who are particularly susceptible to the psychological impacts of frequent medical tests, the use of advanced MRI techniques facilitated by AI can help streamline the imaging process and reduce the burden on families.
The ability to conduct serial MRI scans over extended periods allows healthcare providers to gather critical data for understanding disease progression. Moreover, advancements in AI algorithms that analyze these scans can significantly improve the detection of anomalies, leading to earlier interventions that may enhance the overall treatment trajectory for young patients.
Clinical Trials for AI-Augmented Pediatric Cancer Treatments
The future of pediatric oncology is poised for transformation with the introduction of clinical trials aimed at exploring AI-augmented treatment modalities. These trials seek to validate the efficacy of AI-based predictions in managing pediatric cancer, particularly regarding recurrence rates and treatment efficacy. By integrating cutting-edge AI technology into clinical research, oncologists can refine their approaches to treatment protocols tailored to individual patient profiles.
Initial objectives of these clinical trials include examining whether AI-informed prediction models can significantly reduce the frequency of invasive imaging procedures for low-risk patients while enhancing care pathways for those identified as high risk. This dual approach not only prioritizes patient comfort and well-being but also aims to optimize health resources in pediatric oncology.
Potential Implications of AI in Pediatric Oncological Research
As AI continues to shape the landscape of pediatric oncological research, the possibilities for enhanced understanding of disease mechanisms and treatment responses are immense. The insights drawn from AI analyses not only offer potential for refining current treatment strategies but also hold the promise of discovering novel therapeutic targets based on comprehensive data analytics. The intersection of technology and medicine is paving the way for breakthroughs that could redefine treatment paradigms for pediatric cancers.
Future research will undoubtedly explore the evolving role of AI in understanding the genomic and molecular landscapes of pediatric tumors. By leveraging machine learning alongside large datasets, researchers are better equipped to understand complexities tied to genetic predispositions, which could lead to groundbreaking individualized therapies for young cancer patients.
Families’ Perspectives on AI and Pediatric Cancer Treatment
As technology infiltrates the realm of pediatric oncological care, families of affected children often find themselves navigating new paradigms of diagnosis and treatment. Many families express optimism regarding AI-driven advancements, cherishing the hope that such technologies may lead to improved prognoses and reduced treatment-related challenges. However, they also grapple with navigating the emotional and psychological implications that accompany high-tech medical advancements.
Education and communication play critical roles in bridging the gap between families and the ongoing clinical application of AI tools in pediatric oncology. Ensuring that families understand the fundamentals, benefits, and limitations of AI-enhanced treatments can foster trust and collaboration between caregivers and medical professionals, critical for the holistic care of pediatric patients.
Future Directions for Pediatric Cancer Research and AI
Looking ahead, the integration of AI in pediatric oncology is expected to expand further, with a focus on developing more sophisticated systems that can adapt to the nuanced environments of pediatric care. Research will likely concentrate on creating robust machine learning models that can process a multitude of variables—biological, clinical, and imaging data—to produce more accurate predictions regarding pediatric cancer outcomes and recurrences.
Furthermore, collaborative efforts among institutions will be pivotal in gathering and refining the datasets necessary for training AI models. As larger datasets become available, it is anticipated that these AI systems will equip oncologists with the tools needed to navigate complex treatment landscapes, ultimately leading to better management strategies for pediatric patients and enhanced quality of life.
Frequently Asked Questions
How does AI improve predictions for pediatric cancer recurrence, specifically for gliomas?
AI utilizes advanced algorithms to analyze multiple MRI scans taken over time, enhancing the accuracy of relapse predictions in pediatric cancer patients, particularly those with gliomas. By employing temporal learning techniques, the AI can identify subtle changes in brain scans that indicate potential recurrence, achieving prediction accuracies of 75-89%, compared to only 50% for single-scan assessments.
What role does temporal learning play in predicting pediatric cancer recurrence?
Temporal learning is crucial in predicting pediatric cancer recurrence as it allows AI algorithms to analyze sequential MRI scans instead of isolated images. This approach improves the model’s ability to detect changes over time, which is essential in forecasting relapse risks in conditions like glioma, marking a significant advancement in pediatric oncology.
Why is predicting pediatric cancer recurrence important for patient care?
Predicting pediatric cancer recurrence is vital as it enables targeted follow-up care and therapies. Accurate risk assessments through AI can determine which patients may require more intensive monitoring or intervention, ultimately improving outcomes for children battling pediatric cancers like gliomas and reducing unnecessary stress on families.
What advancements have been made in MRI scans for predicting pediatric cancer recurrence?
Recent advancements in MRI scans for predicting pediatric cancer recurrence include the application of AI and temporal learning techniques. These technologies analyze longitudinal data across multiple scans to enhance prediction accuracy for glioma recurrence, moving beyond traditional models that rely on individual images.
How does AI inform clinical trials for pediatric cancer recurrence risks?
AI informs upcoming clinical trials by providing reliable predictions of pediatric cancer recurrence risks based on analysis of multiple longitudinal MRI scans. Researchers aim to test whether AI-enhanced risk assessments can lead to improved patient care strategies, such as modifying imaging frequency and tailoring treatments for high-risk patients.
What is the significance of machine learning in pediatric cancer diagnosis and recurrence prediction?
Machine learning significantly enhances pediatric cancer diagnosis and recurrence prediction by identifying complex patterns in vast datasets. Its application in analyzing MRI scans leads to better risk stratification for conditions like gliomas, ultimately guiding treatment decisions and improving survival outcomes.
What challenges do families face with pediatric cancer recurrence monitoring?
Families dealing with pediatric cancer recurrence monitoring often face challenges such as the emotional stress of frequent MRI scans and uncertainty about relapse risks. The need for improved prediction methods, such as those developed using AI, aims to alleviate this burden and provide clearer guidelines for follow-up care.
How can improved MRI analysis impact the treatment of pediatric glioma recurrence?
Improved MRI analysis through AI and temporal learning can significantly impact the treatment of pediatric glioma recurrence by accurately predicting relapse risks. This methodology allows for proactive interventions and targeted therapies for high-risk patients, potentially reducing the incidence of devastating relapses.
What future directions are there for AI in the context of pediatric cancer recurrence?
Future directions for AI in pediatric cancer recurrence include further validation of predictive models in diverse clinical settings, integration of AI tools in routine practice, and initiation of clinical trials to assess the impacts of AI-driven care strategies on patient outcomes.
| Key Point | Description |
|---|---|
| AI Tool’s Prediction Accuracy | The AI tool predicts pediatric cancer relapse with 75-89% accuracy, outperforming traditional methods that only achieve about 50% accuracy. |
| Temporal Learning Technique | This method trains AI to analyze sequential brain scans, which improves prediction accuracy of potential relapses in patients post-surgery. |
| Impact on Pediatric Glioma Care | Improved identification of relapse risks could lead to tailored follow-up treatments and reduced imaging stress for patients and families. |
| Study Collaboration | The research was conducted by Mass General Brigham in partnership with Boston Children’s Hospital and Dana-Farber/Boston Children’s. |
| Need for Further Validation | Clinical trials need to be conducted to confirm effectiveness before widespread application of the AI model in medical decisions. |
Summary
Pediatric Cancer Recurrence is a critical area of research, especially for children diagnosed with gliomas. Recent advancements have shown that an AI tool can predict relapse risks more accurately than traditional imaging methods, potentially transforming the management of pediatric glioma. By employing temporal learning from multiple brain scans, this innovative approach allows for earlier identification of patients at high risk of recurrence, thereby improving treatment outcomes and reducing unnecessary stress on young patients and their families. As researchers aim to validate these findings through clinical trials, the future of pediatric cancer care is poised for significant improvements.