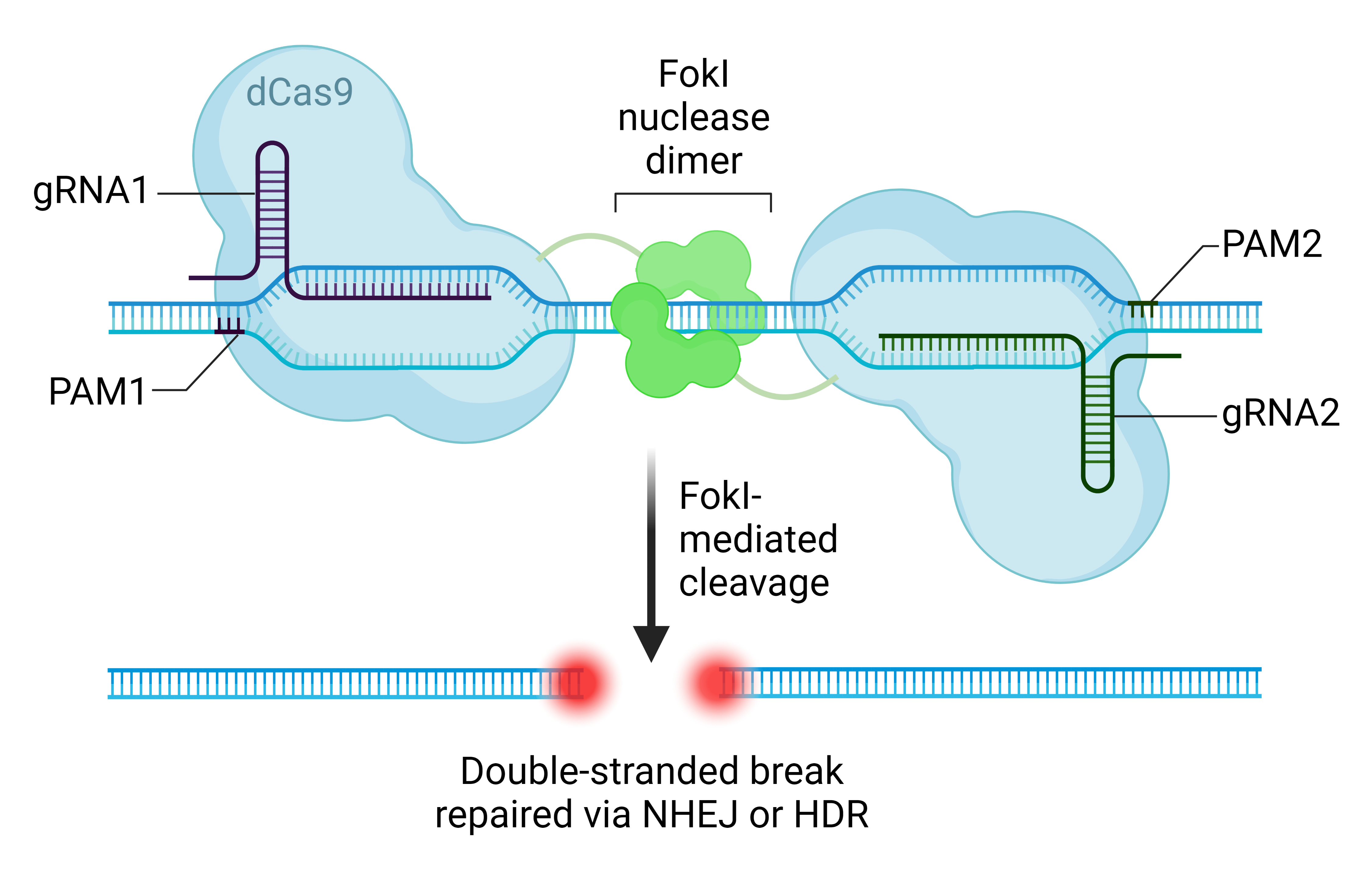
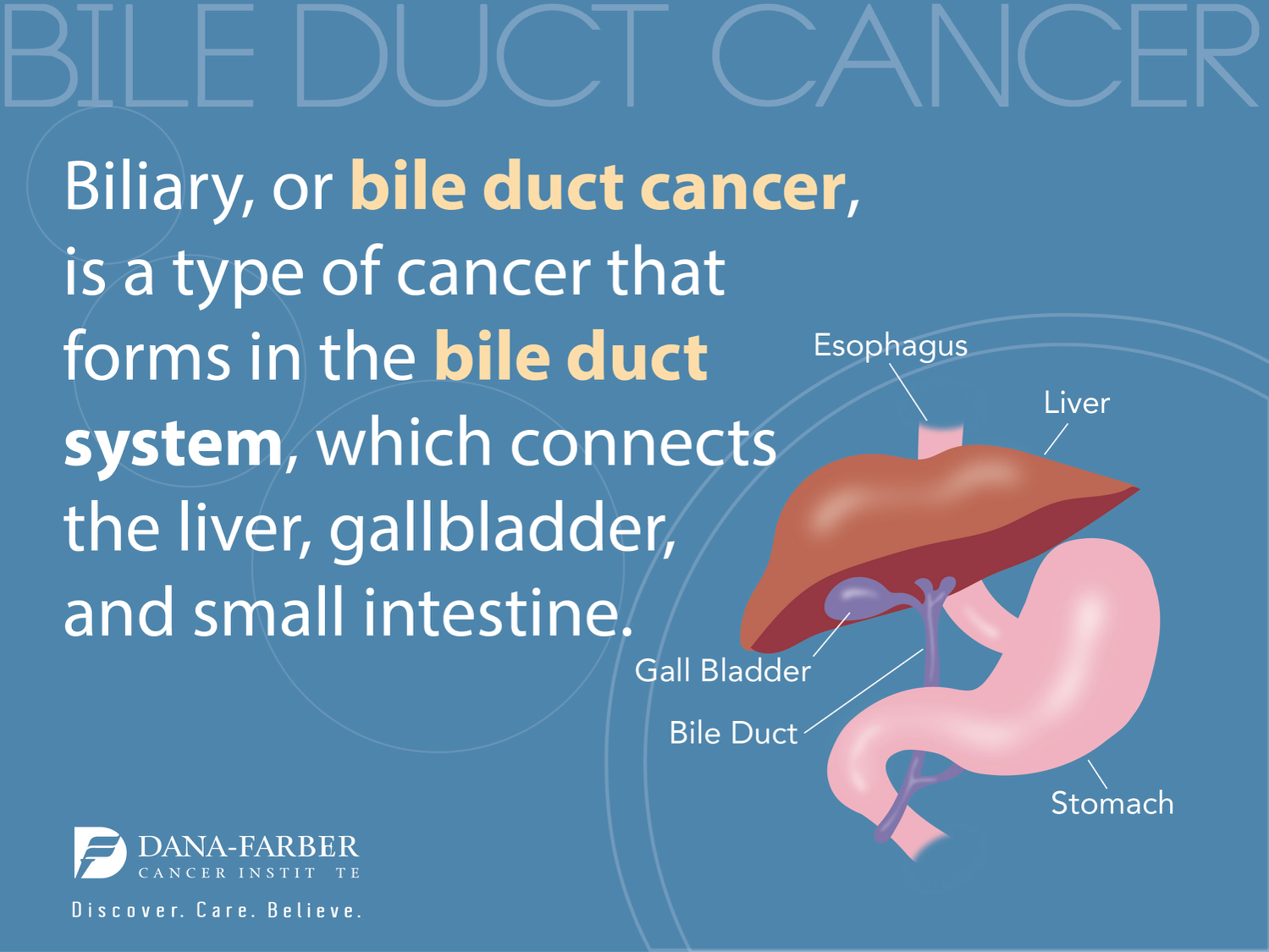
CRISPR gene editing has emerged as a groundbreaking technology that revolutionizes our understanding of genetics and offers the potential to cure devastating diseases like sickle cell anemia. As researchers harness CRISPR technology, they are confronted with complex ethical dilemmas surrounding gene editing ethics and the impacts these new capabilities could have on society. For instance, while the promise of a cure sparks hope for health equity, it also raises questions about who can afford such life-changing interventions. The allure of correcting genetic anomalies must be balanced with serious considerations of bioethics and the long-term implications of such alterations. Ultimately, the conversation about CRISPR gene editing is not just about science; it’s about who we are and what it means to be human in the face of rapid technological progress.
Gene modification techniques, particularly those exemplified by CRISPR gene editing, are at the forefront of medical research, offering tantalizing possibilities for the treatment of genetic disorders. This cutting-edge approach allows scientists to precisely alter DNA sequences, tackling conditions such as sickle cell disease with newfound precision. However, the implications of such technology delve deep into the realm of ethical considerations, with discussions around gene editing ethics ensuring we remain mindful of the societal impacts. As we explore the nuances of bioethics, the challenges of health equity come to light—particularly regarding who benefits from genetic advancements. The journey through gene editing continues to provoke debate about our responsibilities to each other and the future of human genetics.
The Ethical Landscape of CRISPR Gene Editing
The advent of CRISPR gene editing technology heralds a new era in medical science, where the potential to fix genetic disorders raises profound ethical considerations. Experts argue that while the ability to edit genes could eradicate diseases like sickle cell anemia, it also invites scrutiny over the morality of altering human characteristics. The fundamental question emerges: do we have the right to decide which genetic traits are desirable? The implications extend beyond individual choice, touching on societal values and the very fabric of humanity.
Moreover, discussions surrounding CRISPR often highlight a tension between innovation and ethics. As researchers and practitioners like Neal Baer emphasize, the capacity to modify genetic material must be balanced with conscientious reflection on the potential repercussions. For instance, decisions on whether to enhance traits or eliminate conditions that are merely variations of human experience spark debates on the essence of diversity and the acceptance of inherent human differences. This conundrum requires a robust ethical framework to ensure that gene editing practices respect both individual autonomy and collective societal norms.
Addressing Health Equity in Genetic Cures
Health equity is a crucial aspect of the discourse on CRISPR gene editing, particularly when considering the exorbitant costs associated with revolutionary treatments. The case of sickle cell anemia, where the proposed cure can cost upwards of $2.2 million, raises valid concerns about access. Who gets to benefit from these miraculous advancements in medicine? The disparity in healthcare resources globally means that while some may enjoy the luxury of genetic modifications, many others remain deprived of even basic medical care. Such inequalities present a pressing ethical dilemma that must be addressed in the implementation of gene editing technologies.
Furthermore, the conversation around health equity should not only focus on financial implications but also recognize the potential for exacerbating existing health disparities. As Rebecca Brendel points out, without deliberate attention to justice in health innovations, advancements could deepen the divide between those with and without access. Policymakers and scientists are urged to consider how CRISPR can be utilized in ways that promote equitable healthcare access, ensuring that cutting-edge treatments are available to all, not just the affluent. This approach is not only ethical but essential for fostering a just society geared towards the common good.
CRISPR Technology and the Future of Disease Treatment
CRISPR technology holds the promise of revolutionizing disease treatment, enabling scientists to target and repair specific genes responsible for various health conditions. For instance, CRISPR’s ability to edit somatic cells has provided groundbreaking opportunities to treat genetically rooted illnesses like sickle cell anemia. This technology empowers clinicians to intervene at the molecular level, potentially providing lifelong cures for patients who previously faced limited options. However, the journey from lab to patient care is fraught with challenges, including regulatory hurdles and ethical debates about the use of such potent tools.
As we look toward the future, the implications of CRISPR extend beyond mere functionality; they compel us to think critically about gene therapy’s societal impact. Will gene editing become associated with a form of elitism, where only the wealthy can afford safe access? Moreover, the potential for unintended genetic consequences brings forth another layer of complexity, necessitating thorough research before widespread application. With these advancements come a responsibility to guide the conversation about CRISPR technology and ensure its deployment aligns with our ethical commitments to safety, equity, and human dignity.
The Role of Bioethics in Gene Editing
Bioethics plays a pivotal role in navigating the complex terrain of gene editing technologies like CRISPR. These ethical frameworks help to address the myriad of implications associated with modifying human genetics, particularly as advancements unfold at a rapid pace. Deliberations led by bioethicists pose critical inquiries: What constitutes acceptable genetic modification? How do we draw lines between therapeutic and enhancement applications? The establishment of ethical guidelines acts as a safeguard, ensuring that scientific progress does not outpace our moral responsibilities.
Additionally, the integration of bioethical consideration in research and clinical practice fosters a culture of accountability among scientists and healthcare providers. By prioritizing ethical discourse, we can cultivate an environment where the emphasis is not only on innovation but also on the ethical ramifications of our choices. This includes engaging diverse stakeholders in conversations about CRISPR, ensuring that varied perspectives are incorporated into policy-making and practice standards. Ultimately, bioethics equips us with the tools to navigate the nuanced landscape of gene editing responsibly.
Understanding Gene Editing Disparities for Health Justice
Disparities in access to gene editing technology reveal stark contrasts in health justice. As the potential of CRISPR becomes realized, the question of who benefits is more relevant than ever. Systemic inequities can influence who has access to cutting-edge treatments, often aligning with socioeconomic status, geographical location, and race. The discussion must pivot to ensure that the advancements in gene editing do not merely serve to widen existing health divides but instead work to close them. Engaging in dialogues about health equity is crucial to aligning technology with social justice.
To address these disparities, it is essential for stakeholders in healthcare and policy to collaborate effectively. By recognizing and advocating for marginalized communities, we can shape a future in which the benefits of gene editing technologies are more equitably distributed. Initiatives that focus on community outreach, education, and affordable access will be vital in fostering an inclusive approach to gene therapy. This collective effort is not just an ethical obligation but a necessary stride towards achieving health equity in the face of rapidly evolving medical technologies.
CRISPR Innovations and Their Global Implications
The innovations brought forth by CRISPR technology are not merely confined to local advancements; their ramifications echo globally. Efforts to employ gene editing for treating diseases should consider the broader context of healthcare systems worldwide. In countries where resources are scarce, the potential of CRISPR might be perceived as a double-edged sword, raising concerns over the accessibility of such powerful interventions. Global health discourse must anticipate these challenges, navigating the delicate balance between scientific promise and the ethical obligations of ensuring that advancements benefit all of humanity.
Furthermore, the international landscape of gene editing necessitates comprehensive regulations that encompass ethical standards across borders. Just as innovations in CRISPR hold transformative potential, they also invite risks related to unregulated practices. Reinforcing international bioethical guidelines could mitigate concerns regarding misuse or disparity in the experience of gene editing. Through collaboration and shared ethical commitments, researchers and policymakers can foster an environment that respects diverse values and promotes the equitable application of CRISPR technology, paving the way for a future where health innovations lift everyone.
The Future of Genetic Variability in Society
The intersection of CRISPR technology and genetic variability invites profound discourse on our evolving definitions of normalcy and health. As editing techniques become sophisticated, the societal implications of creating genetically modified individuals or populations become increasingly visible. Questions arise around the desirability of certain traits and the potential impact on human diversity. The ability to shape genetic outcomes prompts us to confront what it means to be human and how much we are willing to change ourselves in pursuit of health benefits or societal expectations.
Moreover, there’s an intrinsic value in the variations that exist within our species. Embracing genetic diversity can enrich our collective experience and foster a more inclusive society. As ethicists and scientists consider the role of CRISPR in modifying human traits, they must weigh the benefits of reducing disease against the risk of losing the richness that diversity brings. Future discussions should navigate the potential for gene editing to create a more homogeneous human experience versus honoring our differences as essential characteristics of humanity.
Parenting, Choice, and CRISPR Gene Editing
Gene editing technologies like CRISPR introduce new complexities into the realm of parenting and choice. The decision-making process surrounding genetic modifications for one’s child can evoke strong emotions and ethical dilemmas. Should parents have the authority to decide on genetic traits that align with their ideals of health or ability? Such questions fundamentally challenge the boundaries of parental rights and advocacy for child autonomy. As society grows increasingly capable of customizing genetic outcomes, it is crucial to consider the ethical implications of such choices on the lives of future generations.
Furthermore, the dialogue around CRISPR gene editing also reflects deeper societal values regarding capability and wellness. Parents might be motivated to alter traits out of love and concern for their children, yet these decisions must be weighed against the realities of variation and acceptance within human experiences. The narratives around genetic conditions often underplay the potential for fulfillment and joy, as seen in the example of individuals with conditions like albinism. Advocacy for appreciation and support of diverse human experiences should accompany advancements in gene editing to foster an inclusive outlook that values differences.
Regulatory Frameworks for Safe Gene Editing Practices
As CRISPR technology evolves, the establishment of robust regulatory frameworks is imperative to ensure safe and ethical practices in gene editing. Government and regulatory bodies must work collaboratively with scientific communities to create guidelines that address the multifaceted aspects of gene manipulation. These frameworks should encompass not only the technical safety of treatments but also ethical considerations surrounding consent, access, and the long-term effects of genetic modifications. Legislating responsible practices can safeguard both patients and society from potential misuses of technology.
Moreover, regulatory frameworks should be informed by ongoing public dialogue and engagement. By involving diverse stakeholders, policymakers can better understand the societal implications of CRISPR gene editing. Ethical oversight must include voices from communities that are often overlooked, ensuring that the regulations account for differing values and perspectives. The development of transparent regulatory processes will instill public trust and confidence in gene editing technologies, ultimately guiding their responsible integration into healthcare.
Frequently Asked Questions
What role does CRISPR gene editing play in the cure for sickle cell anemia?
CRISPR gene editing technology has transformed the treatment landscape for sickle cell anemia by allowing scientists to edit the genes responsible for the disease. This technique enables the removal of the defective gene in somatic cells, potentially curing the disease in affected individuals. This advancement raises discussions about the ethics of such interventions and their implications for health equity.
What are the ethical concerns surrounding CRISPR gene editing?
The ethical concerns surrounding CRISPR gene editing include questions of consent, particularly regarding modifications in germline cells that affect future generations. Issues of health equity arise, as expensive treatments may only benefit those who can afford them, leaving marginalized populations without access to potentially life-saving therapies. Additionally, the implications of editing genes for non-life-threatening conditions spark debates on whether we should alter human variation.
How does CRISPR technology contribute to health equity issues in gene editing?
CRISPR technology can enhance health equity by providing cures for genetic diseases like sickle cell anemia. However, the high cost of gene editing therapies, such as the approximately $2.2 million cure for sickle cell, raises concerns about access and fairness in healthcare. If only privileged groups can afford these treatments, disparities in health outcomes may widen, highlighting the need for ethical considerations in the deployment of CRISPR technology.
What are some potential unintended consequences of CRISPR gene editing?
While CRISPR gene editing holds promise for curing diseases, it may also have unintended consequences due to the complex nature of genetics. For example, altering a gene that controls LDL cholesterol can have far-reaching effects on various bodily functions, as genes interact in intricate ways. Careful consideration and regulation are essential to mitigate risks and prevent unforeseen health issues arising from these genetic modifications.
Who is responsible for making ethical decisions regarding CRISPR gene editing applications?
Responsibility for ethical decisions concerning CRISPR gene editing lies with a combination of stakeholders including scientists, ethicists, healthcare providers, policymakers, and society at large. As technology evolves, discussions about who has the authority to decide on the use of CRISPR for certain genetic conditions must involve diverse perspectives to ensure ethical practices that prioritize health justice.
| Key Point | Details |
|---|---|
| Overview of CRISPR | CRISPR is a revolutionary gene-editing technology that allows the modification of both somatic and germline genes. |
| Ethical Concerns | The ability to edit genes raises important ethical questions about human differences and health equity. |
| Costs of Treatment | The cost of gene editing treatments, such as curing sickle cell, can be prohibitively high, around $2.2 million, raising issues regarding who pays for them. |
| Parental Decisions | There are debates on whether parents should have the ability to decide what attributes their children should have through gene editing. |
| Potential for Misuse | Gene editing could lead to unintended consequences, and there are concerns about the lack of monitoring in countries with fewer regulations. |
| Human Variation | Some argue that conditions like deafness should not be viewed as pathologies that need to be ‘fixed’. |
Summary
CRISPR gene editing is a powerful technology that presents both opportunities and ethical dilemmas in medicine. It allows for significant advancements in treating genetic diseases, such as sickle cell anemia, yet poses critical questions about our responsibilities in altering human traits. The discussions around CRISPR echo the need for careful consideration of health equity, parental rights in genetic decisions, and the potential for misuse in various contexts. These conversations are essential as we navigate the future of gene editing, ensuring that innovations are guided by ethical principles and inclusive practices.